Electronic Visit Verification (EVV) was implemented as a result of the 21st Century Cures Act and directs state Medicaid programs to require implementation of EVV for providers of personal care services and home health services.
This new mandate for providers, is confusing to providers who want to understand how billing and claims filing work together with the EVV process. Most providers are comfortable with the compliance piece of EVV and understand the mandatory elements involved including date of service, location of service, individual providing the service, type of service, individual receiving the service and start/end time of the service being provided.
These mandatory requirements go a long way to help reduce fraud and abuse in the Medicaid program; however, a standard EVV program is only one piece of ensuring your claims can and will be paid as a provider.
So how does the process really work to ensure compliance as well as timely and accurate claims payments?
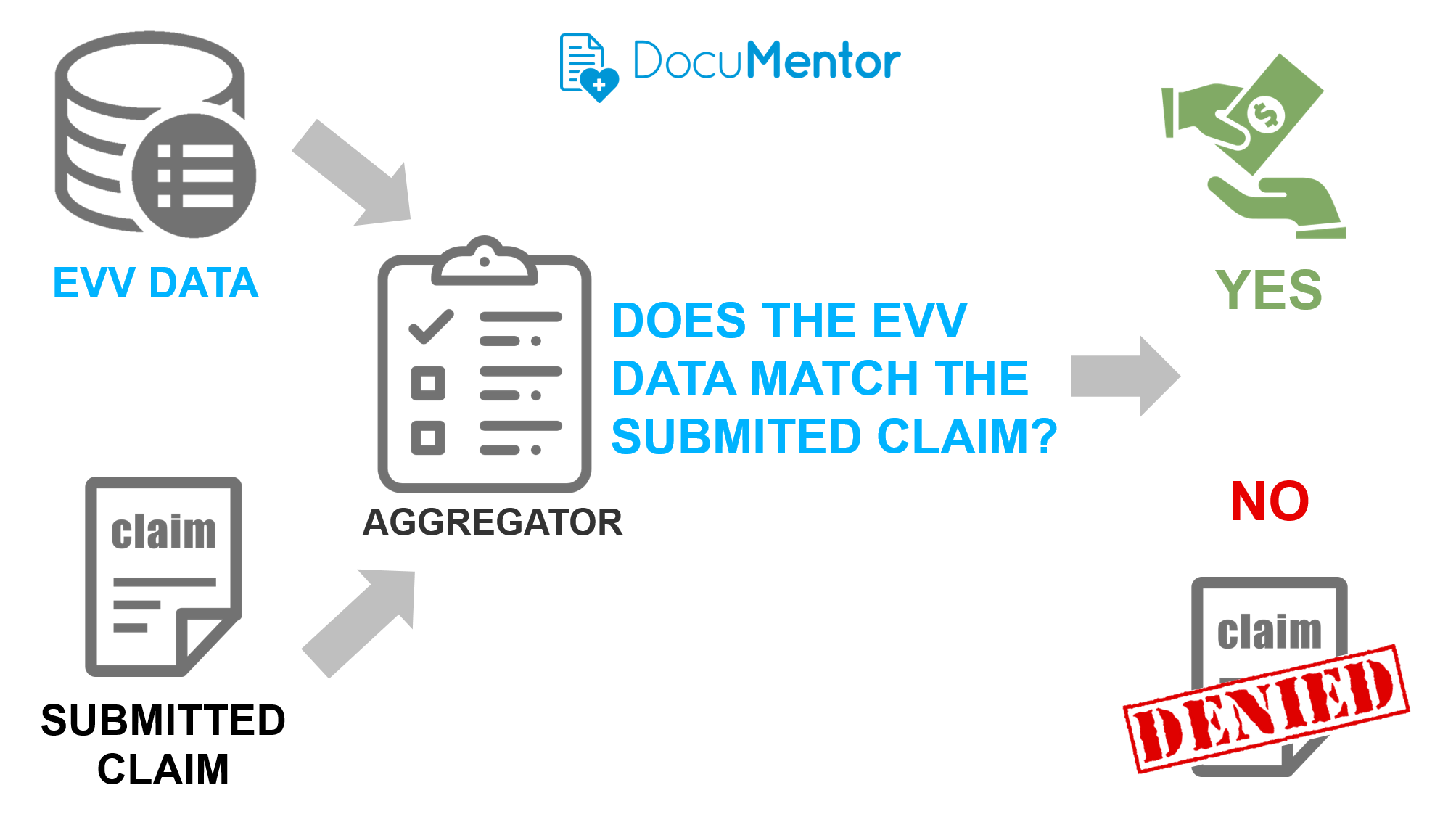
Put simply, states are comparing required data from EVV visits to the claims actually submitted to the state Medicaid aggregator. If the two places do not match then claims will be denied.




